Understanding Ketosis During Acute Illness: An Observational Experience
Ketosis is a metabolic state in which the body shifts from using glucose (sugar) as its primary energy source to metabolizing fat, resulting in the production of ketone bodies by the liver. This process typically occurs in conditions of low carbohydrate availability—such as during fasting, prolonged physical exertion, or carbohydrate-restricted diets.
Food poisoning, by contrast, is an acute gastrointestinal illness caused by the ingestion of food contaminated with pathogenic bacteria, viruses, or toxins. One side effect of food poisoning is reduced food intake, particularly of carbohydrates, due to nausea, vomiting, and general gastrointestinal distress.
Following a suspected incident of foodborne illness—possibly from either contaminated oysters or chicken consumed at a restaurant—I have experienced several days of significantly reduced dietary intake. Since the onset of symptoms, my nutritional focus has been on hydration, electrolyte balance, and gradual reintroduction of easily digestible foods, such as clear soups and bananas, under medical supervision.
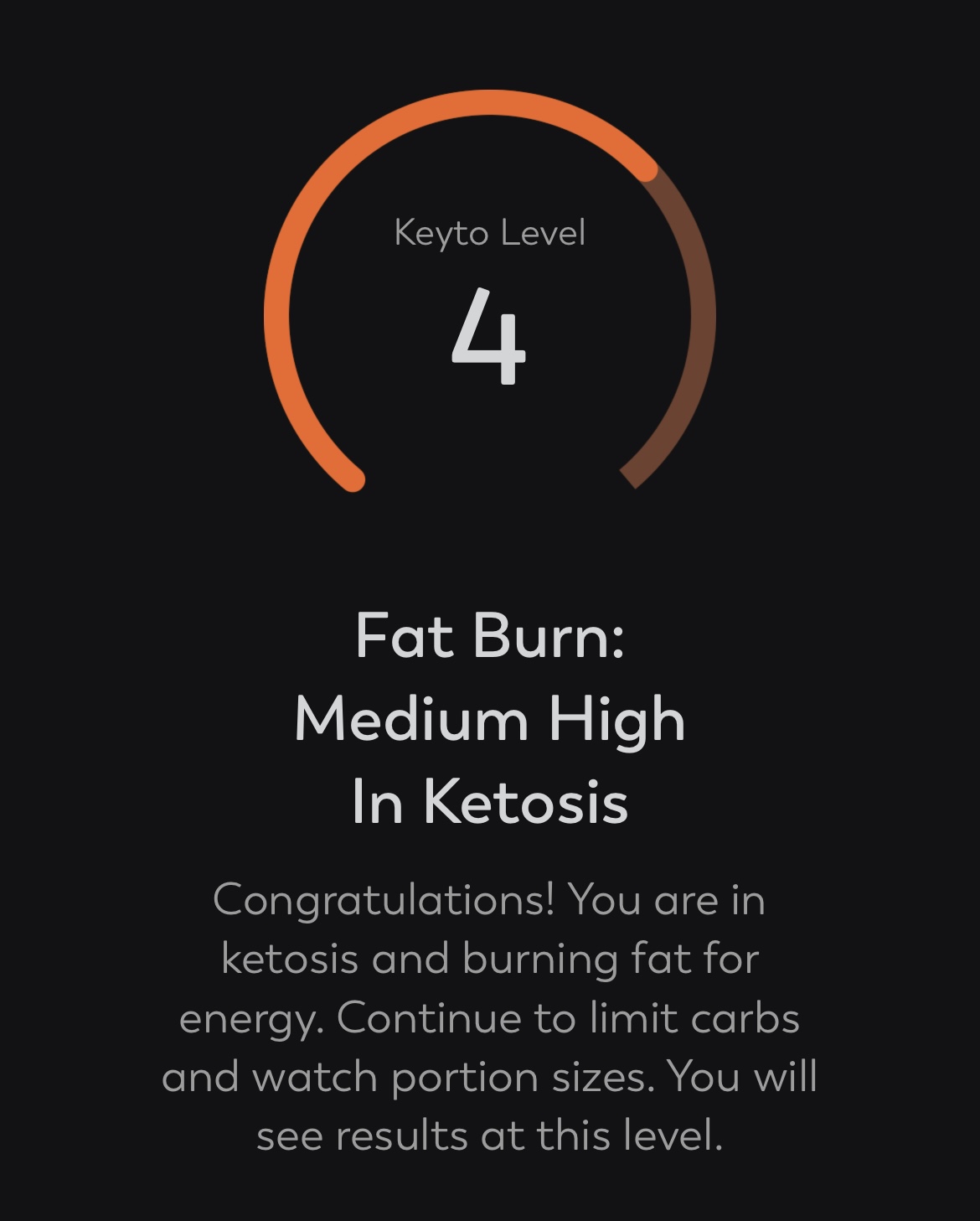
This unintended fasting state has likely induced a medium-to-high level of ketosis, as indicated by physical symptoms and subjective energy shifts. Historically, I have reduced weight safely for athletic competition (Marathon Majors) through controlled caloric restriction, without deliberate use of ketogenic strategies.
Key Observations from Current State:
- Blood Glucose: 3.9 mmol/L, indicative of hypoglycemia.
- Insulin: Not directly measured, but presumed suppressed due to low carbohydrate intake.
- Energy Source: The body has transitioned from glycolysis to lipolysis and ketogenesis.
- Metabolic Process:
- The liver converts stored fat into ketone bodies.
- Ketones are released into the bloodstream and used as an alternative energy source, particularly by the brain.
Symptoms Correlated with Ketosis:
- Halitosis (commonly referred to as “keto breath”)
- Gastrointestinal changes
- Flu-like symptoms (“keto flu”)
- Reduced appetite
- Energy variability and irritability
- Headaches, potentially linked to dehydration
Factors Contributing to Ketosis Induction:
- Carbohydrate intake restricted to near-zero
- High water consumption (approx. 5 liters/day over 2.5 days)
- Electrolyte supplementation (1x Dioralyte daily)
- Continued fluid loss through gastrointestinal illness
- No protein or significant calorie intake
Reflections and Considerations:
This experience, although involuntary, has provided a firsthand perspective on high-level ketosis. I have not previously been able to achieve this state through dietary planning alone, largely due to challenges in managing hunger, energy variability, and physical performance during training.
Interestingly, wearable data (e.g., from WHOOP) has indicated increased physiological strain and stress markers—consistent with illness rather than training adaptation. This highlights a key consideration: while ketosis can amplify fat metabolism, it must be approached with caution. Unplanned or unmanaged ketosis, particularly during illness, can present substantial risks and discomfort.
Conclusion:
While therapeutic or performance-driven ketosis remains a subject of ongoing research and debate, this unintentional induction reinforces the importance of careful nutritional planning and clinical oversight. Further self-study post-recovery may provide more actionable insights, especially regarding the controlled use of light ketosis or intermittent fasting for metabolic benefits. However, this should never be confused with, or replace, safe and balanced nutritional strategies—particularly during periods of compromised health.
Note: This reflection is observational in nature and not intended as medical or nutritional advice.